China’s health sector has made strenuous efforts to improve people’s health over recent decades [25], significantly increasing the strength of public health and the capacity for providing basic medical services and medical security and substantially enhancing physical health and health literacy.
In our study, we determined epidemiological patterns and changes for four categories of bacterial infectious diseases in China by time, region, and population between 2004 and 2019. We found that the incidence of BIDs decreased during the study period, primarily due to reduction in RTDs and DCFTDs. Our data provide evidence that is helpful for clarifying surveillance needs and strengthening BID prevention and control measures.
Although the overall incidence of BIDs decreased, the challenges for BID control are still considerable. Our study showed that tuberculosis still has a high incidence. Northern regions such as Xinjiang had the highest tuberculosis incidence, a phenomenon that may be related to a lower level of economic development and a lack of health education [9]. We also found that the incidence of tuberculosis increased with age, indicating that the elderly were at high risk. To eliminate tuberculosis, strengthening multi-sector cooperation, developing new tuberculosis vaccines, producing new diagnostic and therapeutic drugs, expanding medical insurance coverage, standardizing medical care, and optimizing prevention and treatment strategies are all needed [10].
The incidence of scarlet fever increased fastest among 0‒5- and 6‒14-year-olds, with the highest average annual incidence among six year old children [11]. Children this age are establishing their protective immune functions and may lack immunity against streptococcal infections [12].
Pertussis was decreasing during the first part of the study period, but then began to increase rapidly in all age groups except individuals 65‒74 and over 75-year-olds. One reason for the increase may be waning immunity. Neither natural infection nor vaccination provide lifelong immunity, and people can be infected many times during their life. Vaccine-induced immunity against pertussis is known to wane. Compared with whole-cell pertussis vaccines, acellular pertussis vaccines are less reactogenic and their induced immunity wanes more rapidly [13]. By the second half of the study period, China had switched from whole cell pertussis vaccines to acellular pertussis vaccines. Another potential reason for the increase in pertussis may be evolution of B. pertussis. Emerging B. pertussis lineages (e.g., PtxP3) could be related to the pertussis resurgence [14], as evidenced by the 46.7% prevalence of PtxP3 among isolated circulating strains in Shenzhen [15]. A third possible reason for the increase in pertussis incidence is enhanced B. pertussis surveillance. Medical institutions in many areas have significantly improved their ability and capacity to culture B. pertussis and, especially, to detect pertussis using PCR, resulting in marked improvement in pertussis surveillance sensitivity.
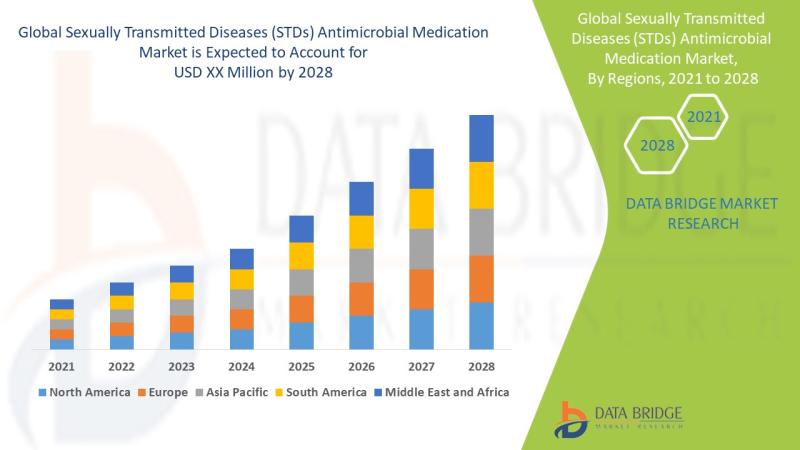
Blood-borne/sexually transmitted diseases incidence increased, with syphilis increasing the most. During 2004‒2006 and 2006‒2010, AAPCs were 35.58% and 19.94%, respectively, but decreased to 3.38% during 2010‒2019. Blood-borne/sexually transmitted diseases incidence, especially syphilis, increased in all seven regions of China, with higher increases in coastal regions and inland border areas of North and Northwest China. As pioneers of economic reform in coastal areas, the rapid development of commercial industries might have led to a higher incidence of syphilis. Sex workers in coastal provinces may have spread syphilis, as has happened in other regions [16]. Syphilis increased the most in relative terms among individuals 65‒74 and over 75-year-olds (AAPC, 17.46%, 14.66%). Syphilis increased in other age groups as well (except for 0-5-year-olds). The increasing incidence of syphilis may also be due to expansion of syphilis screening. Joint screening of HIV and syphilis with voluntary counselling at testing clinics expanded screening, as did preoperative screening for syphilis. Western lifestyles and cultures, including more open discussion about sex, are prominent in Chinese social media [17]. Therefore, Chinese people are more tolerant of a variety of sexual behaviors. In 2010, China promulgated a national syphilis prevention and control program (2010‒2020) [18], which could have been the key driver that slowed the increasing incidence of syphilis that was seen in 2010–2019. The large disease burden of syphilis in China demands more epidemiological investigation, increased screening, expanded partner services, more effective behavioral interventions, and multi-sectoral commitment [19].
Zoonotic and vector-borne diseases incidence increased, mainly due to increases in brucellosis. During 2004‒2014, the incidence of brucellosis increased by 13.20% per year. In the early part of the study period, brucellosis was most prominent in the northern pastureland provinces that practiced animal husbandry and therefore had more opportunity to contact infected livestock. There was also increased attention paid to brucellosis with strengthened brucellosis surveillance. In recent years, transporting animals from different regions led to importation of brucellosis into the southern region [20, 21]. China initiated the National Medium and Long-term Animal Disease Prevention and Control Plan (2012‒2020) and the National Disease Control Plan (2016‒2020), which, together, likely led to the decline in the incidence of brucellosis. After 2014, the incidence decreased by about 7.47% per year. The northern region still has a higher incidence than other regions. To reduce brucellosis, it is important to enhance vaccination of livestock such as cattle and sheep, reduce occupational exposure, and conduct health education for populations at risk of exposure [2].
Etiological diagnosis is essential for clinical management of infectious diseases and for monitoring and providing early warning of infectious diseases [22]. The diagnostic laboratory capacity for infectious diseases in primary medical institutions is insufficient in China. Insufficiency may be due to financial constraints of central medical institutions or a low technical capacity. Therefore, construction of the infectious disease monitoring laboratory network should be further strengthened [23, 24].
Our study had several limitations. First, the data were from NIDRIS, which may lack representativeness with underreporting of BIDs. Second, we did not calculate temporal trends for all BIDs. Age-specific trends of leprosy and cholera could not be calculated with joinpoint regression due to too few cases. Third, multi-drug resistant TBC is an important public health issue. Since July 1, 2017, the “Infectious Disease Reporting Information Management System” has adjusted the TB classification, adding “Rifampicin resistance” to the TB classification. However, due to the small number of reported cases and the short reporting period, no separate study was conducted in this study.
In conclusion, our study showed that incidences of BIDs declined, especially RTDs and DCFTDs, but tuberculosis incidence stayed high. BSTDs and ZVDs increased, but as we adopted control measures against these diseases, the growth in incidence decelerated. We should pay more attention to BIDs, strengthen active monitoring, construct laboratory networks, and adopt timely control measures to reduce the incidence of infectious diseases in China.
Discovered on: 2023-05-02 00:00:00
Source: Incidence and trends of 17 notifiable bacterial infectious diseases in Chin…