A new study has shown that taking a single dose of a widely used, cheap antibiotic within 3 days after condomless sex can help prevent chlamydia, syphilis, and gonorrhea, three sexually transmitted infections (STIs, also referred to as sexually transmitted diseases or STDs) that have soared in the United States, Europe, and elsewhere over the past 2 decades.
The study, mainly in men who have sex with men (MSM) in San Francisco and Seattle, was halted in May after an independent data monitoring board found that the strategy, known as doxycycline postexposure prophylaxis (doxyPEP), reduced the risk of chlamydia and gonorrhea by more than 60%—a result so convincing there was no need to continue the study. DoxyPEP also appeared to protect against syphilis, but too few cases occurred during the trial to reach statistical significance. The data were scheduled to be presented this week at the 24th International AIDS Conference in Montreal.
“This is very encouraging,” says Carlos del Rio, an HIV/AIDS clinician and researcher at Emory University School of Medicine. But there are worries the regimen could trigger antibiotic resistance in the three bacteria that cause these diseases, and scientists are divided about whether the data warrant doxyPEP’s introduction now. “It is still a controversial topic,” says Jean-Michel Molina of the University of Paris Cité, who led a similar, smaller study in France a few years ago. “I don’t think we know enough to recommend the strategy yet.”
Doxycycline, a relative of the antibiotic tetracycline, has been around for more than 45 years and is commonly used to treat and prevent acne and Lyme disease. It also acts on parasites and is widely prescribed to prevent malaria in travelers. The drug typically has few side effects beyond stomach upset and increased sensitivity to sunlight.
Preventing bacterial STIs in MSM has become more important in part because of the success of antiretrovirals against HIV, which has led to more condomless sex. The drugs can lower the levels of the virus in infected people so substantially that they rarely transmit it and can also protect uninfected people who take them regularly before sex as pre-exposure prophylaxis (PrEP).
The idea for the new doxycycline study comes from a small trial published in 2015. Fifteen MSM, who were at high risk of STIs because of their sexual behavior and already took medications for their HIV infections, added the antibiotic to their daily pill regimen. When compared at 48 weeks with 15 similar MSM not given the antibiotic, the men who took doxycycline as PrEP had significantly fewer infections with all three bacterial STIs. “That was promising—as a pilot study,” says Jeffrey Klausner, an infectious disease specialist at the University of Southern California who co-led the trial.
Molina’s study in France, published in 2018, was based on the same idea, but with a slight difference: Doxycycline was used as PEP, not PrEP. Participants took the drug once, within 72 hours after having condomless sex. The team found this reduced the risk of acquiring chlamydia or syphilis by 70% and 73%, respectively, but there was no effect on gonorrhea rates.
The new study enrolled 544 participants—mostly MSM, but also some transgender women and gender diverse people—deemed at high risk for STIs. Two-thirds of them were asked to follow a protocol similar to the one in the French study. The remaining participants received standard STI testing and treatment. Everyone knew what group they were in. “We really wanted to do a study in a fairly real-world setting,” says one of the principal investigators, Annie Luetkemeyer, an infectious disease clinician at the University of California, San Francisco.
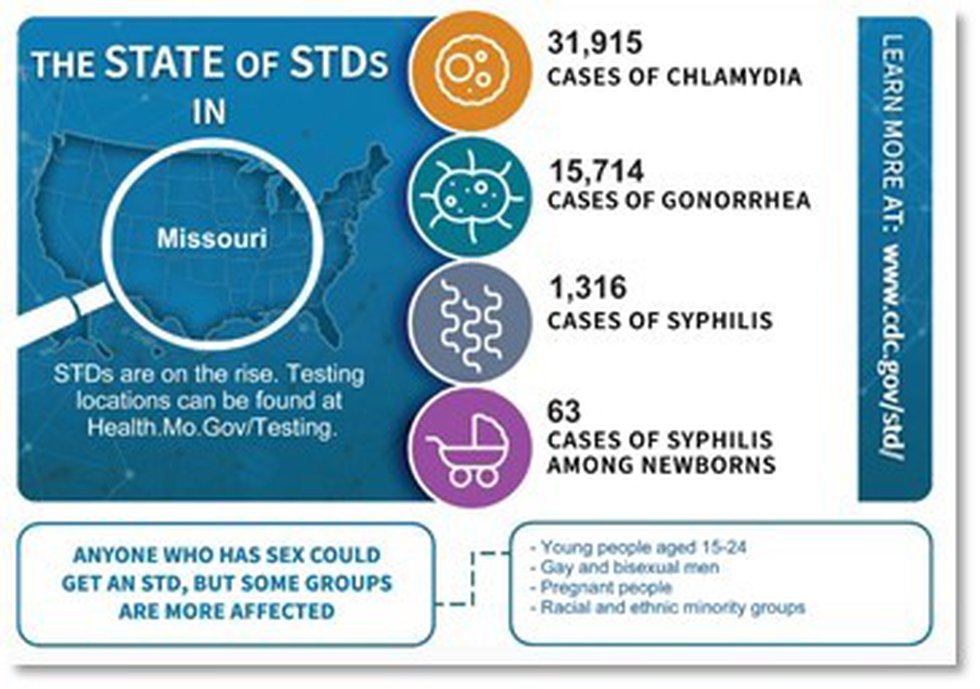
Growing problem
Annual U.S. cases of three sexually transmitted infections caused by bacteria have risen sharply in the past 2 decades.
(GRAPHIC) K. FRANKLIN/SCIENCE; (DATA) U.S. Centers for Disease Control and Prevention
Leandro Mena, who heads the division of the U.S. Centers for Disease Control and Prevention (CDC) that oversees STIs, says he is “very excited” about the findings. “We want to have the opportunity to fully review the data,” Mena says, but CDC may soon issue preliminary guidance about the regimen for high-risk populations.
Researchers differ on whether doxyPEP’s benefits outweigh the risk of driving antibiotic resistance. Neisseria gonorrhoeae, unlike the bacteria that cause the other two STIs, readily develops resistance. (Molina suspects doxyPEP failed against gonorrhea in France because 81% of the participants at the study’s outset had resistance to it—about twice the prevalence seen in the new study.) DoxyPEP will make that worse, Molina predicts—“That’s a no-brainer.” What will happen with chlamydia and syphilis, which have not yet evolved to resist antibiotics, “we don’t know—we hope,” he says.
The U.S. team is still analyzing antibiotic resistance data from its study. But even if doxyPEP increases resistance in N. gonorrhoeae, it won’t have a practical impact because a different antibiotic class is now used to treat gonorrhea, notes Connie Celum, an epidemiologist at the University of Washington, Seattle, and one of the principal investigators. “I really don’t see that as a major downside,” she says. Besides, doxyPEP would only be recommended for people at high risk of STIs, a relatively small group, she says.
Celum is also involved in a doxyPEP study of Kenyan women who take PrEP for HIV and have disproportionately high rates of STIs. “We need interventions now, and this is a safe, inexpensive, well-tolerated drug that really seems to have few downsides,” she says. And treating those at highest risk may help reduce the spread of the STIs in the wider population, Celum adds.
The strategy may have other downsides, however, notes Christopher Fairley, who heads the Melbourne Sexual Health Centre at Monash University, Clayton. Antibiotics can disrupt the bacterial microbiome in the gut, for example, and resistance genes can jump between bacteria. Many gonorrhea and chlamydia infections cause no symptoms, resolve without treatment, and are “of no great significance,” he adds. (Untreated syphilis, in contrast, can damage the eyes, ears, and brain, and can lead to miscarriage and stillbirth in pregnant people.)
But Klausner says the benefits outweigh the risks. Some physicians who treat MSM already prescribe doxycycline for STI protection, he notes. “Patients in the community know about it,” he says. “The time is now to come up with recommendations.”
Discovered on: 2022-10-13 00:00:00
Source: Taking an antibiotic after sex could help curb three common STDs | Science