In the Central Valley, where two-thirds of the nation’s fruit and nuts are grown, the pastoral landscape masks entrenched racial and economic disparities. Life expectancy in Fresno County, for example, drops by 20 years depending on where you live, and it’s those who live in historically poor, redlined or rural neighborhoods who are most impacted by a resurgence of maternal and congenital syphilis.
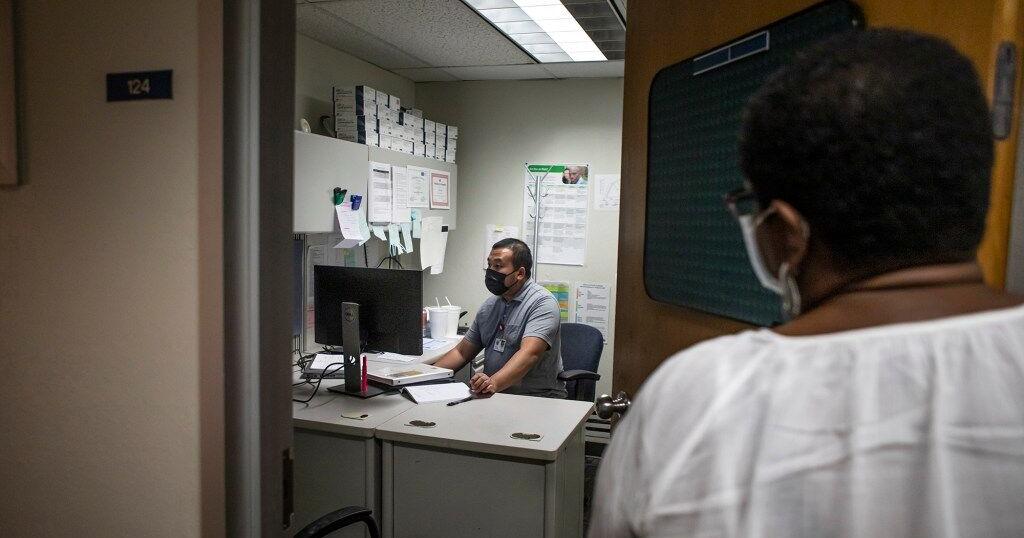
“Are you familiar with syphilis?” Hou Vang, a county communicable disease specialist, asks a pregnant woman standing in the shade of a tree outside her home.
She lives with her parents in Reedley, California, a small town 30 minutes southeast of the city of Fresno, surrounded by neat rows of grapevines, orange groves and almond trees.
“I mean, you hear things,” she says, distractedly eyeing a family member’s car pulling into the driveway. The woman allowed CalMatters to report on her diagnosis on the condition of anonymity.
“It’s an STD (sexually transmitted disease). We like to disclose in-person in case there are any questions,” Vang says. “You did test positive.”
“Oh my God,” she breathes, tearing up. “I have a lot of questions for my kid’s dad.”
Vang works for the county health department, where he’s on the front lines of California’s fight against maternal and congenital syphilis. Rates of infection have ballooned to numbers not seen in two decades. Congenital syphilis occurs when the infection is passed from mother to baby during pregnancy. If untreated, the infection has devastating consequences, causing severe neurological disorders, organ damage and even infant death. In few places is it worse than California’s Central Valley.
Today, California has the sixth-highest rate of congenital syphilis in the country, with rates increasing every year. In 2020, 107 cases per 100,000 live births were reported, a staggering 11-fold increase from a decade prior. That rate far exceeds the California Department of Public Health’s 2020 target to keep congenital syphilis numbers below 9.6 cases per 100,000 live births — a goal it outstripped almost as soon as it was set.
Even more shockingly, the syphilis rate among women of childbearing age was 53 times higher than the 2020 goal.
At one point in the late 1990s, rates were so low across the country that the Centers for Disease Control and Prevention thought syphilis among men and women could be effectively eradicated from the population. After all, in many cases a single shot of penicillin is all that’s needed to curb the infection. But at both the national and state level, public health departments were overstretched and woefully underfunded. People slipped through the cracks, and sexually transmitted infections of all types began to skyrocket once more.
Increasing case rates have also gone hand-in-hand with increasing rates of homelessness and methamphetamine use. Inadequate prenatal care is the No. 1 predictor for maternal and congenital syphilis. It is a disease whose reemergence signifies severely inadequate access to health and social services systems.
“When they rank developed nations on health measures, the indicators always include sexually transmitted diseases,” said Dr. Mohammad Nael Mhaissen, a pediatric infectious disease specialist at Valley Children’s Hospital in Madera. “And we’re failing.”
This should ‘never’ happen
Vang knows when he has found a meth den. The sharp, acrid scent of the drug is unmistakable — it smells like cat pee.
He’s had doors slammed in his face and a gun flashed at him once. He takes it all in stride, accepting that many people are wary when a government vehicle pulls up in front of their home. His job is to track down people who have tested positive for sexually transmitted infections, and his most urgent cases are pregnant women who have syphilis.
Medical historians call it “the great imitator” because the symptoms are commonplace and disappear after a few weeks even though the body still carries the bacteria. Women in particular may never notice the painless bumps of early infection until it comes back months or years later to wreak havoc on their internal organs. Too often, women aren’t diagnosed until they’re well into their pregnancy, when the infection can cause severe physical and cognitive disabilities for the baby, attacking their bones and nervous system. If untreated, there’s a 40 percent chance the baby will die.
In 2019, the most recent year detailed state data is available, 37 syphilis babies were stillborn and 446 were infected. Black babies were three times more likely to be born with syphilis compared to the statewide rate, while Hispanic babies made up nearly 50 percent of all cases. (Native American infants were not included in this calculation because numbers are too low to be statistically stable.)
It can be easy to blame women’s choices for increasing rates, but the truth is much more complicated. The CDC noted in its 2020 Sexually Transmitted Disease Surveillance report that “these disparities are unlikely explained by differences in sexual behavior and rather reflect differential access to quality sexual health care.”
Dr. Dominika Seidman is an obstetrician and gynecologist with Team Lily at UC San Francisco. Her group provides prenatal care and wraparound social supports such as housing navigation, substance abuse and mental health treatment for vulnerable women.
For a long time there were no cases in San Francisco, Seidman said. In 2020, there were five, but the low numbers are misleading. Even one case of congenital syphilis is known as a “sentinel event” in health care — an event so rare and preventable that its occurrence should ring alarm bells.
“This should be a never event,” Seidman said. “It is an absolute disgrace that we are even talking about congenital syphilis.”
It’s hard to pinpoint one reason for the resurgence of this and other sexually transmitted infections, which have also reached record-setting numbers, but high on the list is barriers to health care. In a recent study led by state health department researchers, babies born in the poorest census tracts in the state experienced congenital syphilis at 17 times the rate of those born in the most affluent census tracts.
“This is a reflection of holes in our safety net, and it’s a reflection of all the different social determinants of health that play into poor health outcomes,” said Dr. Ina Park, medical director for the California Prevention Training Center at UC San Francisco and co-author of the CDC’s 2020 sexually transmitted infection treatment guidelines. Park was not involved in the study.
Those social determinants of health — or barriers such as housing instability or lack of insurance — lead to missed opportunities to stop the infection from spreading. In the first two years of California’s outbreak, between 2012 and 2014, nearly one-third of mothers who gave birth to babies with syphilis were never tested before delivery and one-third were tested less than 40 days before giving birth. In contrast, every mother who gave birth to syphilis-free babies was tested early in their pregnancy, according to state researchers.
Those disparities haven’t budged in the ensuing years. In 2018, more than half of pregnant women with syphilis had delayed or no prenatal care, according to a more recent analysis from the California Department of Public Health. Half reported methamphetamine use, and roughly half were recently incarcerated or homeless, the report said.
“It is structurally a socioeconomic issue — a race issue,” said Jennifer Wagman, a UCLA researcher who in 2018 oversaw a study in Kern County aimed at identifying why women were missing prenatal care.
“We’re not seeing wealthy white women with (congenital syphilis) babies. It’s just not happening,” Wagman said.
In the Central Valley in particular, language and distance create additional barriers.
One woman whom Wagman interviewed for her study said “You don’t make it to the appointments because it’s going to take too long on the bus or you won’t make it back in time to pick up the kids at school. You know transportation is a big, big issue.”
This is certainly true of Vang’s latest case in Reedley. He assures the woman that the infection is curable and that it’s lucky it was caught relatively early in her pregnancy, in her second trimester. But her case is complicated. She’s allergic to penicillin, the primary treatment option, and will have to be gradually desensitized to the antibiotic over time. She also has a seizure disorder and can’t drive, relying on family members for transportation. The only hospital that can treat her is Community Regional Medical Center in downtown Fresno, 30 minutes away.
“That’s a far drive. Plus the time for desensitization. That’s a whole day not only for her but for whoever drives her,” said Vang’s boss, Jena Adams. “That’s a barrier.”
They offer her a $20 ARCO gas card and $20 Walmart card per treatment in hope that it will help offset the cost of transportation.
Discovered on: 2022-10-10 22:00:00
Source: STD rate soars across Central Valley, state as public health funding dwindl…